Unrelated mortality after endoscopic eradication of Barrett's neoplasia
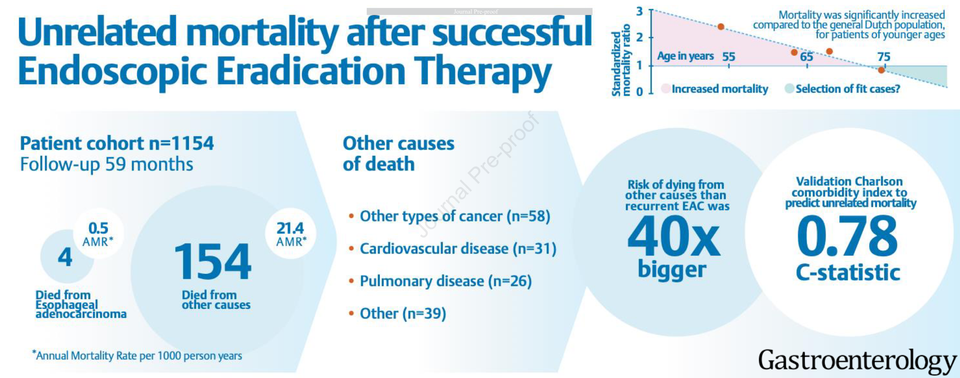
This study provides valuable context for patients and their physicians concerned about future health implications of their diagnosis and treatment for Barrett's neoplasia (dysplasia or early cancer.) It investigates the risk of mortality unrelated to esophageal adenocarcinoma (EAC) in patients who have undergone endoscopic eradication therapy (EET) for Barrett’s neoplasia, combining data from a nationwide registry in the Netherlands with national mortality statistics to accurately assess mortality rates.
The findings reveal that the risk of mortality from causes other than EAC (e.g., various cancers, cardiovascular and pulmonary diseases) is substantially (40 times) higher than the risk of EAC-related mortality, particularly among younger patients. For reference, the IC-RISC™ (“Interactive & Contextual RISk Calculator”) provides mortality rates for selected causes of death in the U.S. specific for age and sex in black males, white males and white females.
Moreover, the study demonstrates that the Charlson Comorbidity Index (CCI), a widely used scoring system that predicts long-term mortality risk based on comorbidities and age, is effective in forecasting mortality in this patient population.
Overall, the study underscores the necessity of incorporating the risk of mortality from unrelated causes into post-EET follow-up protocols and emphasizes the utility of the CCI in predicting individual mortality risk. These findings provide valuable insights for developing more personalized management approaches for patients undergoing EET for Barrett’s neoplasia.
Comments? tvaughan@uw.edu
Incidence and prediction of unrelated mortality after successful endoscopic eradication therapy for Barrett’s neoplasia.
Gastroenterology (2024), doi: https:// doi.org/10.1053/j.gastro.2024.02.033
van Munster SN, Verheij EPD, Ozdemir Ö, Toes-Zoutendijk E, LansdorpVogelaar I, Nieuwenhuis EA, Cotton CC, Weusten BLAM, Alvarez Herrero L, Alkhalaf A, Schenk BE, Schoon EJ, Curvers WL, Koch AD, de Jonge P-JF, Tang TJ, Nagengast WB, Westerhof J, Houben MHMG, Shaheen NJ, Bergman JJGHM, Pouw RE.
Abstract
Background and aims: Follow-up (FU) strategies after endoscopic eradication therapy (EET) for Barrett’s neoplasia do not consider the risk of mortality from other causes than esophageal adenocarcinoma (EAC). We aimed to evaluate this risk during long-term FU, and to assess whether the Charlson Comorbidity Index (CCI) can predict mortality.
Methods: We included all patients with successful EET from the nationwide Barrett-registry in the Netherlands. Data were merged with National Statistics for accurate mortality data. We evaluated annual mortality rates (AMR, per 1000 person-years) and standardized mortality ratio (SMR) for other-cause mortality. Performance of CCI was evaluated by discrimination and calibration.
Results: We included 1,154 patients with a mean age of 64 years (±9). During median 59 months (p25-p75 3791; total 6,375 person-years), 154 patients (13%) died from other causes than EAC (AMR 24.1 [95%CI 20.5-28.2]), most commonly non-EAC-cancers (n=58), cardiovascular (n=31), or pulmonary diseases (n=26). Four patients died from recurrent EAC (AMR 0.5 [95%CI 0.1-1.4]). Compared to the general Dutch population, mortality was significantly increased for patients in the lowest three age quartiles (i.e. age <71 years). Validation of CCI in our population showed good discrimination (C-statistic 0.78 [95%CI 0.72-0.84]) and fair calibration.
Conclusion: The other-cause mortality risk after successful EET was more than 40 times higher [48; 95% CI 15-99] than the risk of EAC-related mortality. Our findings reveal that younger post-EET patients exhibit a significantly reduced life expectancy when compared to the general population. Furthermore, they emphasize the strong predictive ability of CCI for long-term mortality after EET. This straightforward scoring system can inform decisions regarding personalized FU, including appropriate cessation timing. (NL7039)
