Indicators of prognosis among patients with esophageal adecnocarcinoma
Dr. Matt Buas and colleagues analyzed clinical and lifestyle factors among 371 persons with esophageal adenocarcinoma. A number of factors correlated with improved survival, depending on stage. Among those with localized or regional tumors, smoking was associated with a 2.5-fold increased mortality.
Cancers (Basel). 2021 Sep 16;13(18):4653.
Clinical and Lifestyle-Related Prognostic Indicators among Esophageal Adenocarcinoma Patients Receiving Treatment at a Comprehensive Cancer Center
Shruti G Dighe 1 , Li Yan 2 , Sarbajit Mukherjee 3 , Cailey S McGillicuddy 1 , Karen L Hulme 1 , Steven N Hochwald 4 , Saikrishna Yendamuri 5 , Andrew J Bain 3 , Kevin T Robillard 3 , Kirsten B Moysich 1 , Christine B Ambrosone 1 , Amy E Millen 6 , Matthew F Buas
PMID: 34572881
Abstract
Purpose: The incidence of esophageal adenocarcinoma (EAC) has risen substantially in recent decades, while the average 5-year survival remains only ~20%. Disease stage and treatment are the strongest prognostic factors. The role of lifestyle factors in relation to survival remains uncertain, with a handful of studies to date investigating associations with obesity, smoking, physical activity, diet, or medications.
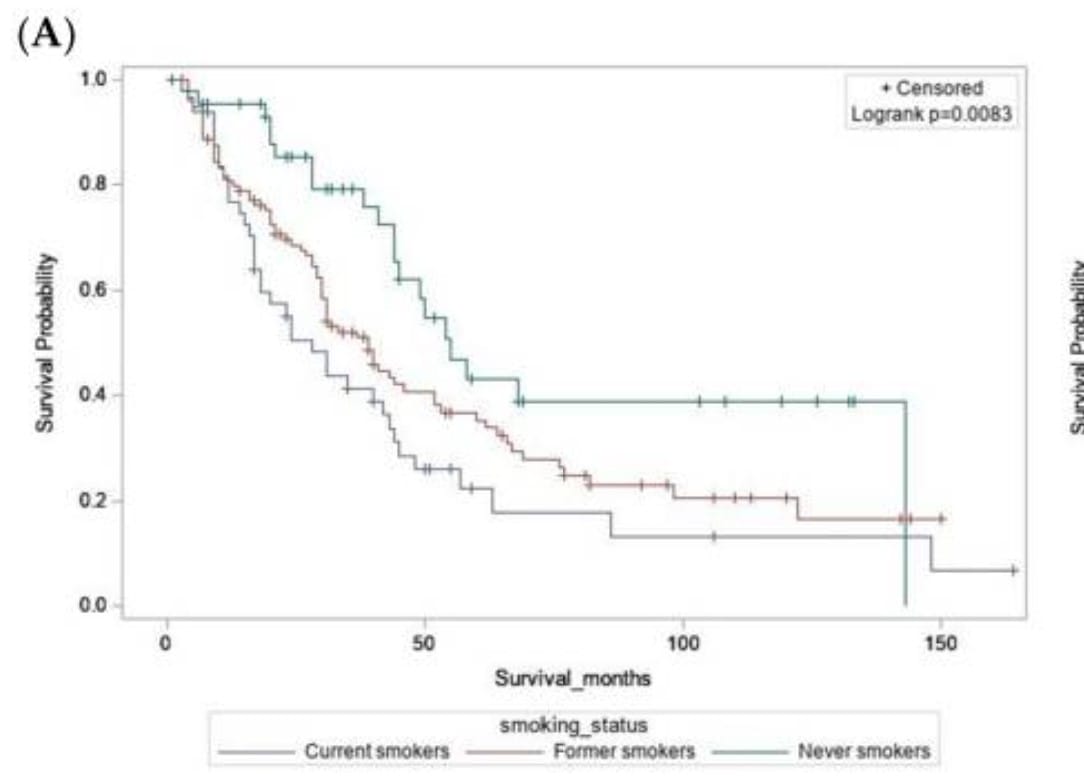
Methods: This study included patients diagnosed with primary adenocarcinoma of the esophagus, gastroesophageal junction, or cardia (N = 371) at Roswell Park Comprehensive Cancer Center between 2003 and 2019. Leveraging extensive data abstracted from electronic medical records, epidemiologic questionnaires, and a tumor registry, we analyzed clinical, behavioral, and environmental exposures and evaluated stage-specific associations with survival. Survival distributions were visualized using Kaplan-Meier curves. Cox proportional hazards regression models adjusted for age, sex, stage, treatment, and comorbidities were used to estimate the association between each exposure and all-cause or cancer-specific mortality.
Results: Among patients presenting with localized/regional tumors (stages I-III), current smoking was associated with increased overall mortality risk (HR = 2.5 [1.42-4.53], p = 0.002), while current physical activity was linked to reduced risk (HR = 0.58 [0.35-0.96], p = 0.035). Among patients with stage IV disease, individuals reporting pre-diagnostic use of statins (HR = 0.62 [0.42-0.92], p = 0.018) or NSAIDs (HR = 0.61 [0.42-0.91], p = 0.016) had improved overall survival. Exploratory analyses suggested that high pre-diagnostic dietary consumption of broccoli, carrots, and fiber correlated with prolonged overall survival in patients with localized/regional disease.
Conclusion: Our data suggest that lifestyle exposures may be differentially associated with EAC survival based on disease stage. Future investigation of larger, diverse patient cohorts is essential to validate these findings. Our results may help inform the development of lifestyle-based interventions to improve EAC prognosis and quality of life.