Sleep apnea and BE
This provocative study, while based on a chart review, suggests that persons with obstructive sleep apnea have a three-fold increased risk of BE even after controlling for obesity and reflux symptoms.
J Gastroenterol Hepatol. 2019 Jul 10. doi: 10.1111/jgh.14779. [Epub ahead of print]
Independent association of obstructive sleep apnea with Barrett’s esophagus.
Hadi YB1, Khan AA1, Naqvi SFZ1, Kupec JT1.
Abstract
BACKGROUND AND AIM:
Current guidelines suggest screening at-risk groups of patients for Barrett’s esophagus (BE), a precursor to esophageal cancer. Although BE and obstructive sleep apnea (OSA) have common risk factors, including elevated body mass index and gastroesophageal reflux disease (GERD), the relationship between these two conditions has not been well established.
METHODS:
Retrospectively, all patients who had undergone a polysomnography and esophagogastroduodenoscopy at West Virginia University Hospital from 2013 to 2018 were identified and divided into groups on the basis of the presence or absence of OSA. Clinical course and procedure reports were reviewed to identify relevant variables.
RESULTS:
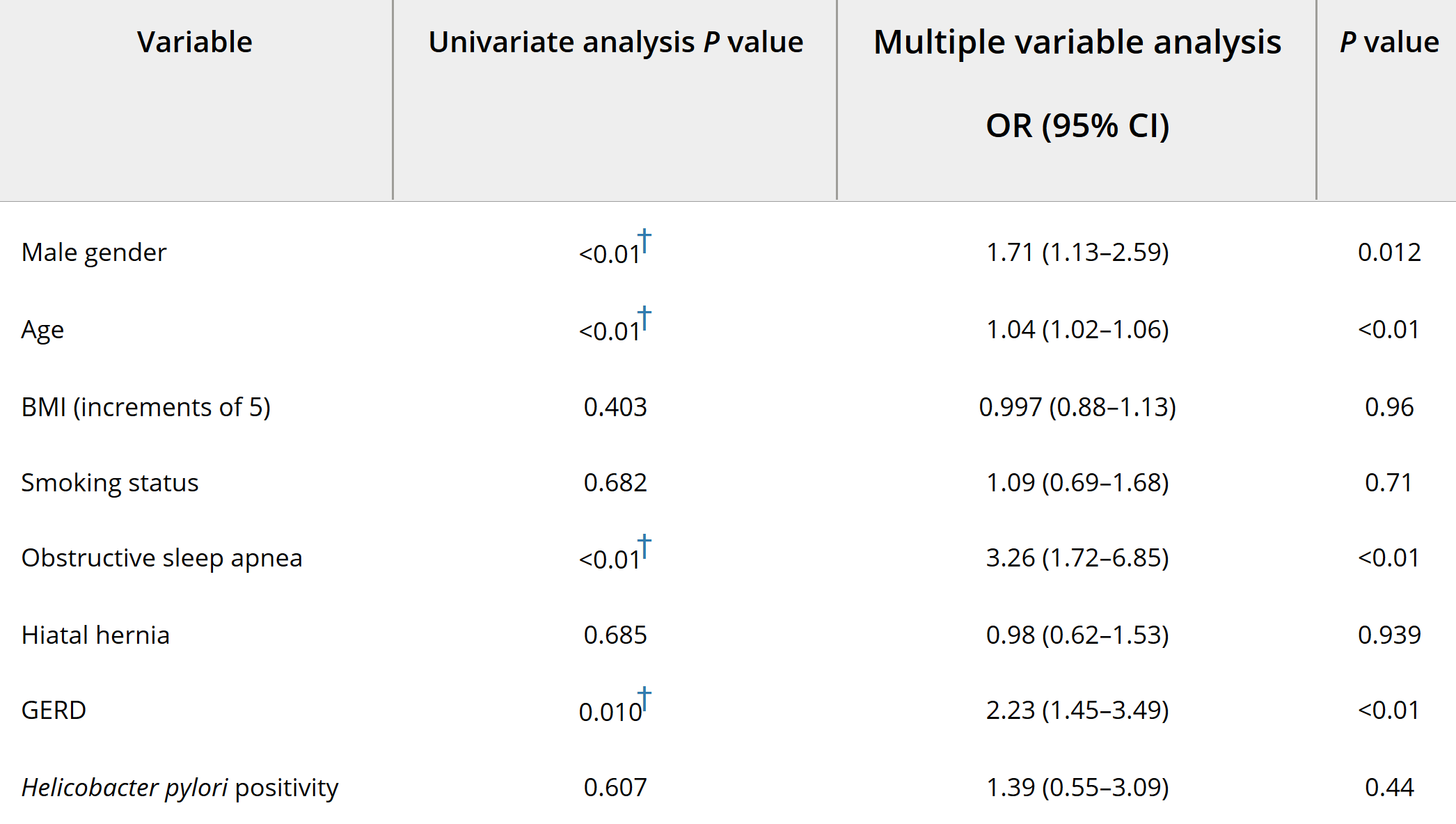
One thousand ninety-one patients met inclusion criteria; 60.9% were female, and mean age of participants was 53.5 years. Univariate analysis revealed that male gender, age, diagnosis of OSA, severity of OSA, and a clinical diagnosis of GERD were associated with BE (P values < 0.05). Multiple logistic regression incorporating age, sex, clinical diagnosis of GERD, smoking history, body mass index, Helicobacter pylori status, and presence of hiatal hernia was utilized. Patients with OSA had an increased risk of BE than had those without OSA (P < 0.001, odds ratio 3.26 [1.72-6.85]). The risk increased with increasing severity of OSA, categorized in apnea-hypopnea index increments of 10.
CONCLUSION:
Obstructive sleep apnea is associated with BE, a relationship that is independent of other known risk factors. Additionally, this risk increases with increasing severity of OSA. Future efforts should determine if patients with severe OSA need to be screened for BE due to its potential for causing esophageal cancer.