Tension between risk-based and patient-centered esophageal cancer screening
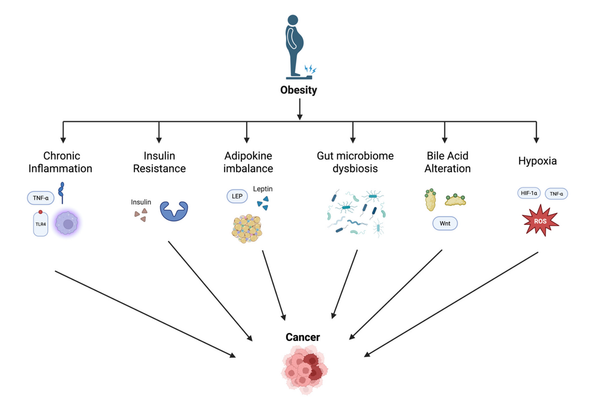
This interesting and thoughtful paper by Dr. Elspeth Davies at the University of Cambridge investigates the use of the capsule sponge test for screening Barrett's esophagus (BE) in a mobile clinic in England, highlighting the challenges in balancing patient-centered and risk-centered medical management. Through ethnographic fieldwork, the study reveals that while the test aims to identify cancer risk, patients often seek reassurance or immediate symptom relief, while a BE diagnosis can lead to persistent anxiety about cancer. The research underscores the need for healthcare to address both the emotional and psychological needs of patients alongside medical risks, and suggests that changing the terminology around BE could help reduce fears and promote a hopeful outlook on cancer prevention. The author summarizes:
Even as medical practice becomes increasingly oriented towards potential futures described by statistics, current embodied experiences remain important to people who become patients. In the case of the capsule sponge test, offering information on symptom management was one way of mediating this tension between ‘patient-centred care’—concerned with the needs of the individual—and risk-centred care—primarily concerned with the statistical risk of disease. Like in other screening programmes, there remain questions about the value of screening people who are at low risk of cancer but who desire reassurance.
‘This has given me the peace of mind I needed’: ethnographic insights into Barrett’s oesophagus screening using the capsule sponge test
Davies E.
J Med Ethics 2024; doi:10.1136/jme-2024-109928
Abstract
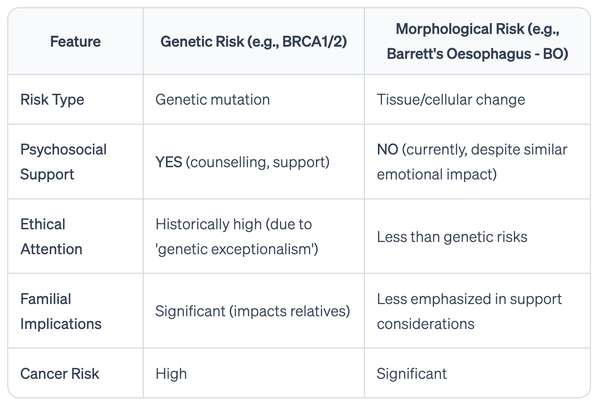
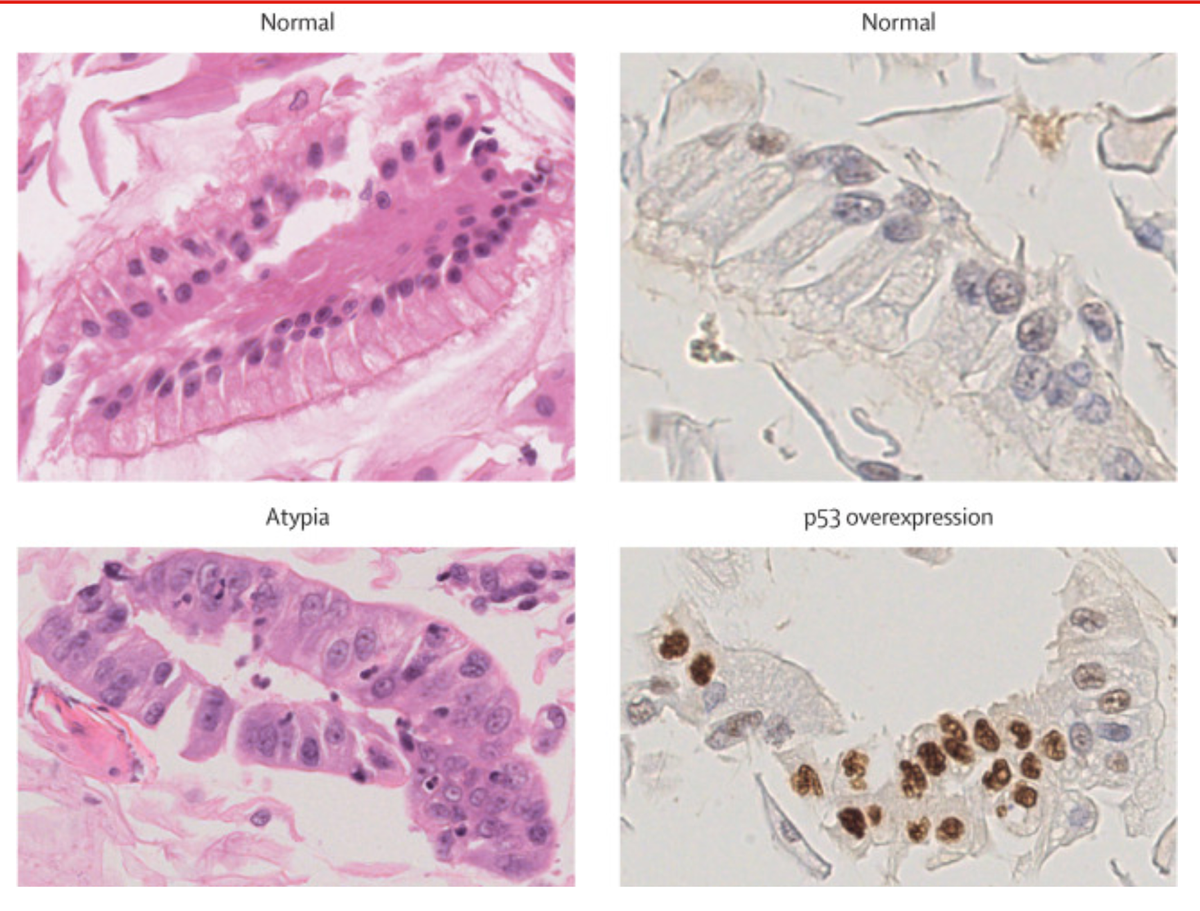
In 2021 and 2022, researchers carried out an implementation trial that considered how the capsule sponge test might be used to screen for Barrett’s oesophagus using a mobile clinic in East Anglia. This paper offers insights from 15 months of ethnographic fieldwork studying the trial. It aims to highlight the value of the test in offering reassurance to worried patients, particularly to those with a family history of oesophageal adenocarcinoma. It also considers the variety of aims people held for the capsule sponge test, including the hope that it would address their symptoms of acid reflux, and the conflict that sometimes emerged as a result. The second half of the paper uses fieldwork carried out in virtual support groups for people with Barrett’s oesophagus to explore experiences postdiagnosis, which sometimes were defined by fear of future cancers. It describes notable differences between the care offered to people with morphological risk conditions like Barrett’s oesophagus and the care given to those with genetic risk conditions, including the provision of genetic counselling. More broadly, the paper highlights a tension between patient-centred and risk-centred medicine that is likely to grow as healthcare services continue to shift towards preventative approaches.